Experts from the African region has projected that the integration of hepatitis in the health systems, can be eliminated with adequate funding and vaccination by 2030.
This was made known on Monday at the World Health Organisation side meeting of the African Hepatitis Summit for new guidelines dissemination.
According to them, viral hepatitis infection is a global public health and development issue, and Africa is greatly affected with more than 91 million Africans living with viral hepatitis B and C.
The WHO further said an estimated 1.2 million new hepatitis infections and 125,000 hepatitis-related deaths occurred in the African region in 2019.
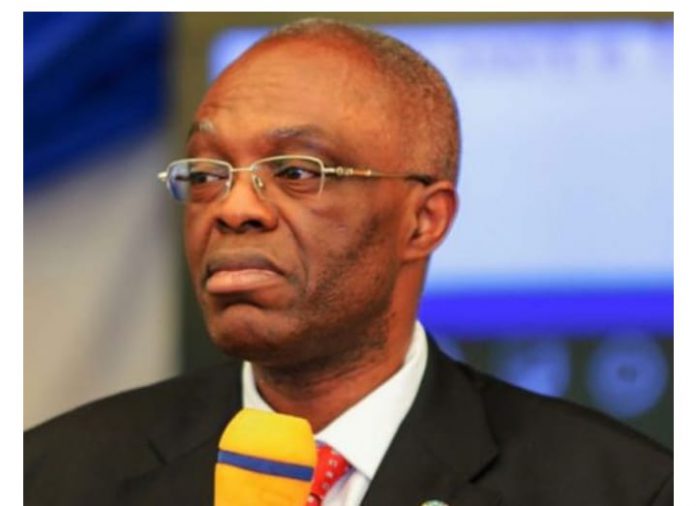
Speaking at the meeting, WHO’s Country Representative, Dr. Walter Mulombo, said that despite available diagnostic tools and effective treatment, less than 10 per cent of the population in Africa are aware of the infections and more than 90 percent of people living with hepatitis in the region do not receive the care they need, leading to progressive advanced liver disease, devastating financial burden, and other effects.
Mulombo, who was represented by the deputy country representative, Dr. Alexander Chimbaru, said countries in the region must take advantage of available tools and interventions to ensure liver health for everyone.
He further called on the member states in the African region to implement the WHO framework and the guidelines.
“WHO’s global hepatitis strategy which has been endorsed by all WHO member states, and the framework for an integrated multisectoral response to TB, HIV, STIs, and hepatitis in the WHO African region serves to provide clear guidance and interventions to reduce new hepatitis infections by 90 per cent and deaths by 65 per cent by 2030 using a public health approach.
“We are looking at the elimination of hepatitis by 2030 but for that to happen, we need all the politicians, the communities, the policymakers, and all the partners to support this. We need to look at how best to bring communities on board to make sure that we defeat hepatitis.
“Nigeria has the potential to achieve the 2030 target because the infrastructure, the politicians, the communities are on board to control the disease but we need to follow the guidelines provided by the government to achieve the target. We have some ongoing programmes like HIV control, and hepatitis control and that means we can leverage the existing platforms in controlling the disease,” he stated.
The Hepatitis Focal Point in the Africa regional office of the WHO, Dr. Casimir Manzengo said 82 million Africans are living with hepatitis B while nine million Africans live with hepatitis C, but only five per cent of them are aware of their status.
He said, “So, they can’t access the treatment and that is why we are motivating our colleagues to advocate with the national authority to make the services more available for the patients.
“Another thing is that we need to increase the vaccination birth dose. Until now, we have just 15 countries in the African region that have integrated hepatitis birth dose vaccination, countries need to prioritise this so we can avoid this infection at birth and the consequences like cirrhosis and cancer.
“We need to have a common integrated process of planning, we should plan for HIV, TB, and hepatitis at the same time. So when we are advocating for HIV funding, we can also have some funds for hepatitis. We should advocate to the authority level, it is better to have some funds in the hand before going to the partners to ask for funding.”
Also, the WHO team lead for hepatitis, Prof. Olufunmilayo Lesi said if no action is taken to eliminate the disease, the death rate from hepatitis B and C will exceed that of HIV and malaria by the year 2040.
Lesi said if Egypt can achieve the gold tier status on the path of eliminating hepatitis C, then other African countries can achieve it.
“There are challenges and one of them is funding. It will cost about 8bn for the global response and a lot of cost is for the commodities -test kits and the drugs.
“Another challenge is political will. Hepatitis must be a public health approach, it means that it is not in the consulting clinics or tertiary centres, but it must come to general hospitals and primary healthcare.
“The political will is important, and the national planning and the coordination of the response are important. This has been done for HIV and it can be done for viral hepatitis and we can make it by integrating it into existing systems,” she said.